What Are Glucocorticoids Used For
- Current issue
- Advance articles
- Volume 18; 2022
- Volume 17; 2021
- Volume 16; 2020
- Volume 15; 2019
- Archive
- Cover images
- Index & coverage
- Cover proposition
- Special issues
Int J Biol Sci 2021; 17(six):1530-1537. doi:10.7150/ijbs.58695 This issue
Review
Glucocorticoids are double-edged sword in the treatment of COVID-19 and cancers
Department of Full general Surgery of Ruijin Infirmary, Shanghai Institute of Digestive Surgery, and Shanghai Key Laboratory for Gastric Neoplasms, Shanghai Jiao Tong University School of Medicine, 200025, Shanghai, Mainland china.
This is an open admission article distributed under the terms of the Creative Eatables Attribution License (https://creativecommons.org/licenses/by/4.0/). Encounter http://ivyspring.com/terms for total terms and conditions.
Citation:
Yang R, Yu Y. Glucocorticoids are double-edged sword in the treatment of COVID-19 and cancers. Int J Biol Sci 2021; 17(6):1530-1537. doi:10.7150/ijbs.58695. Bachelor from https://www.ijbs.com/v17p1530.htm
Abstract
Glucocorticoids are important steroid hormones. As an outstanding scientific discovery, the scientist who discovered glucocorticoids was awarded the Nobel Prize in Physiology and Medicine in 1950. Cortisone (hydrocortisone) is a natural glucocorticoid, which is secreted with cyclic rhythm by the cortical cells of adrenal glands. Physiologically, about 10-20 mg of hydrocortisone are secreted each day for maintaining homeostasis. Since the biological half-life of natural glucocorticoid is short, scientists developed various synthetic glucocorticoids including prednisone, prednisolone, methylprednisolone, triamcinolone, dexamethasone, betamethasone, and then on. These synthetic glucocorticoids are generated past modifying some structures based on the cortisone courage, leading to extension of their biological half-life with stronger activities. In the confront of astringent infection, allergy, stupor, trauma, pain, and other stresses, the demand for glucocorticoids increases dramatically. It is critical to supplement extra glucocorticoids to protect the biological functions of vital organs. However, the corporeality and duration of glucocorticoid administration need to be carefully adjusted, because a series of side effects may occur later on long-term or high-dose usage of glucocorticoids. This review commodity volition hash out the application of glucocorticoids in the treatment of patients with astringent or critical COVID-19 and solid tumors of advanced stage. The controversy of using glucocorticoid in medical customs will also be discussed. This review article volition aid doctors and basic researchers meliorate empathise the practical application of glucocorticoids.
Keywords: COVID-xix, Therapy, Glucocorticoids, Cancer
Classification of glucocorticoids
The discovery of glucocorticoid (cortisone) was awarded the Nobel Prize in Physiology and Medicine in 1950. Glucocorticoids are stress response hormones that bind to glucocorticoid receptor, and play disquisitional roles in various physiological processes such as metabolic homeostasis, knowledge, cell proliferation, reproduction, and inflammation. Glucocorticoid receptor (GR) belongs to the steroid-thyroid-retinoic acid nuclear receptor superfamily. In the absence of glucocorticoid binding, GR resides in the cytoplasm inactively binds to heat-stupor proteins, FKBP51 and FKBP52. Upon glucocorticoid binding, GR undergoes conformational changes, dissociates from the chaperone proteins, and translocate into the nucleus, where it binds to promoter Deoxyribonucleic acid of target genes, resulting in stimulation or suppression of the transcription of response genes. Natural glucocorticoids, namely cortisone or hydrocortisone, are cholesterol-derived hormones secreted by the adrenal glands and are named afterward their roles in maintaining glucose homeostasis. The release of glucocorticoids into blood circulation has systemic roles in allowed response, metabolism, cell growth, development, and reproduction. Attributable to their anti-inflammatory and immune-suppressive actions, glucocorticoids are among the near unremarkably prescribed drugs. Some autoimmune, inflammatory, and allergic disorders, including rheumatoid arthritis, lupus erythematosus, inflammatory bowel illness, transplant rejection and asthma are oft treated with glucocorticoids [one, ii]. Therefore, glucocorticoids are considered every bit a standard handling in the in a higher place-mentioned diseases. Physiologically, an developed secretes ten-xx mg of glucocorticoids per 24-hour interval with circadian rhythms. The peak secretion is in the 6:00 to 8:00 a.m. The secretion of glucocorticoids are regulated by hypothalamic corticotropin, and secreted by adrenal cortex. In the face up of stress, such every bit infections, trauma or surgery, the serum cortisol level could be increased to up to 150-200 mg. Since the cortisol was first synthesized in 1948, studies have been carried out with the aim of synthesizing steroids with a specific anti-inflammatory action [iii]. Pharmacological dose of glucocorticoids plays roles on anti-inflammation, anti-allergy, anti-shock, and immunosuppression. The medication of glucocorticoids should be given in accordance with the cyclic rhythm in the early on morning. Regarding the effect of anti-inflammation, glucocorticoids can quickly inhibit transcription of inflammatory cytokines, including IL-2, IL-3, IL-four, IL-5, IL-half-dozen, TNFα, GM-CSF, CCL1, CCL5, CCL11, and CXCL8 et al.[iv].
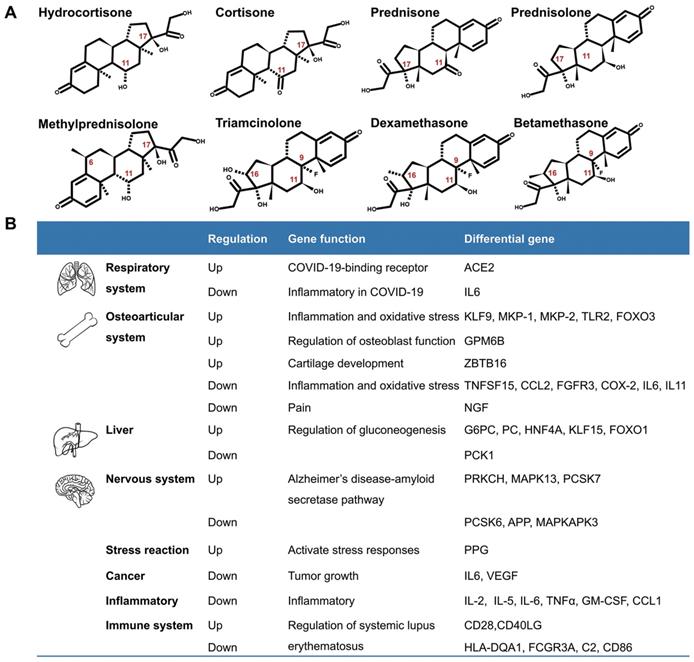
Although glucocorticoids have different names, they accept similar biological effects. The usually used glucocorticoids are prednisone, prednisolone, triamcinolone, methylprednisolone, dexamethasone, and others. They are modified in the chemical structures of the cortisone (hydrocortisone) backbone in social club to enhance their anti-inflammatory effects. The chemical modifications include introduction of 6α-fluoro commutation, and reducing the binding to the mineralocorticoid receptor by insertion of a C=C double bond at C1, C2, or replacing a lipophilic substituent such every bit 21α-esters attached to the D-ring for increasing binding to glucocorticoid receptors [5] (Fig.1A). According to their duration of activity, glucocorticoids are divided into short-acting, mid-interim, and long-interim drugs. The biological half-life of cortisone (hydrocortisone) is 8-12h, that of prednisone, prednisolone, methylprednisolone, and triamcinolone is 12-36h, and the biological one-half-life of dexamethasone and betamethasone is 36-54h (Table 1)[6-8]. The administration routes of glucocorticoids include external use, inhalation, oral and injection.
Glucocorticoids and GR take been an of import expanse of research because of their pleiotropic physiological functions and extensive use in clinics. A number of genes are regulated by glucocorticoids (Fig. 1B). Recently, Pemmari and colleagues examined the global gene expression profiles of chondrocytes that were treated with dexamethasone for 24h past RNA-Seq. They found that dexamethasone affected lipid and glucose metabolism-related genes in add-on to their anti-inflammatory, anticatabolic, and extracellular matrix-targeting effects [nine]. In human, many inflammatory genes are downstream genes of glucocorticoids. Escoter-Torres and Grbesa systematically summarized target genes based on glucocorticoid-GR binding. The broad physiological effects of glucocorticoid on the nervous (beliefs, anxiety, visual), cardiovascular, immune, respiratory, reproductive, and musculoskeletal systems besides as on metabolism take been introduced [10]. The well understanding of these genes will be helpful for proper usage of glucocorticoids [eleven].
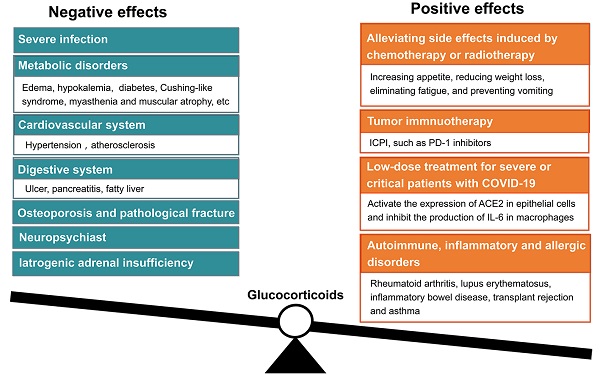
Double-edged sword concerns about glucocorticoids
Glucocorticoids are one of those medications that are regularly prescribed in both inpatient and outpatient departments. Their anti-inflammatory activity is generally used in treating various conditions, such as allergy, asthma, arthritis, inflammatory bowel illness, and cancer metastasis or exacerbation. However, they accept numerous side effects, such as fluid retentiveness, weight proceeds, and hyperglycemia, et al. With the long-term usage of glucocorticoids, specially long-term loftier-dose applications, a serial of adverse events would appear. These adverse events include osteoporosis, hyperglycemia, insulin resistance, hypertension, muscle cloudburst, severe infection, Cushing-like syndrome, peptic ulcers, and neuropsychiatric disorders. Actually, it is a real practical skill of a medico to be able to properly apply glucocorticoids. Cortisone (hydrocortisone) is physiologically similar to the internal hormone, and mainly used in the alternative treatment of adrenal insufficiency and other endocrine diseases. Considering the stronger anti-inflammatory effect and longer biological half-life, prednisolone, or methylprednisolone are mainly used in the handling of rheumatoid immunologic diseases. Prednisone must be converted into prednisolone in liver, therefore, prednisolone should be chosen to avoid depression treatment efficacy if patients have abnormal liver function. In critical conditions, such every bit sepsis, severe asthma, severe drug rashes, and acute nephritis, high doses of glucocorticoids are used intravenously. Glucocorticoids could not exist used as elementary antipyretic analgesic drugs. Glucocorticoids should exist given locally when patients present with local inflammation, i.e., intra-joint injection is used for the handling of arthritis, inhalation for asthma, and local application for dermatitis. The anti-inflammatory activities of classical glucocorticoids are useful for brusk-term use in near patients, but their chronic and systemic use unremarkably causes side furnishings, and results in reducing sensitivity. The agin effects of glucocorticoids are usually associated with high dose and long duration usage. Mazzantini and coworkers institute that the handling with x mg/d prednisone or equivalent for more than iii months leads to a 7-fold increase in hip fractures and a 17-fold increment in vertebral fractures. Glucocorticoids are the most common cause of secondary osteoporosis, and so-chosen glucocorticoid-induced osteoporosis [12]. In add-on, high dosage of glucocorticoids is immunosuppressive and can increase the risk of fatal infection. Therefore, giving optimal dosage of glucocorticoids at the right fourth dimension is vital to command homeostasis, and avoid detrimental immunosuppression [13].
Fig 1
Introduction of glucocorticoids. A. The chemical structure of common glucocorticoids. B. The genes regulated by glucocorticoids in respiratory arrangement, osteoarticular system, liver, nervous system, stress reaction, cancers, inflammation, Alzheimer disease and systemic lupus erythematosus, et al.
(View in new window)
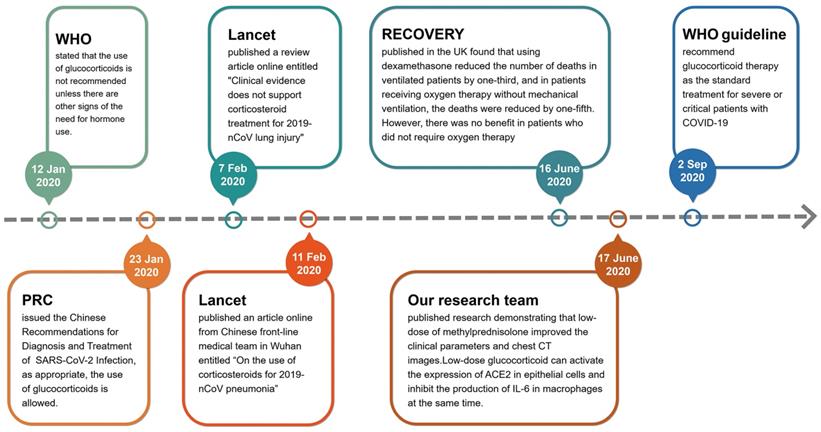
Glucocorticoids and COVID-19 therapy
In the early stages of the outbreak of COVID-nineteen in Wuhan, Prc, glucocorticoids were used cautiously. On 12 January 2020, the World Health Organization (WHO) issued the provisional guidelines for the treatment of severe acute respiratory infections suspected of 2019-nCoV, which stated that the use of glucocorticoids is not recommended unless there are other signs of the demand for hormonal use (https://world wide web.who.int/publications/i/detail/10665-332299). On 7 February 2020, the Lancet published a review article online entitled "Clinical evidence does non back up corticosteroid handling for 2019-nCoV lung injury"[14], only four days subsequently, the Lancet published another commodity online from Chinese front-line medical team in Wuhan entitled "On the use of corticosteroids for 2019-nCoV pneumonia"[xv]. Obviously, the use of glucocorticoids in the treatment of critical COVID-19 cases at the early stage of pandemic is controversial. According to the ongoing theory, glucocorticoids are the most important regulatory hormones in stress response. When a patient is faced with a serious stress like COVID-19, it is hard for doctors to avoid using glucocorticoids [sixteen]. Therefore, doctors in various countries initiated a number of clinical trials to assess the efficacy of glucocorticoids [17-23]. On 23 Jan 2020, the National Health Commission of PRC issued the Chinese Recommendations for Diagnosis and Treatment of Severe Novel Coronavirus (SARS-CoV-2) Infection (Trial version), which proposed that the use of glucocorticoids is allowed if appropriate (http://www.nhc.gov.cn/yzygj/s7653p/202001/9fbefc9a5fe747e98ea5baeedfb68158.shtml). The results of clinical trials on the benefits of using glucocorticoids in the treatment of patients with COVID-xix were gradually published in mid-2020. The most famous clinical trial result of Randomised Evaluation of COVID-19 Therapy (RECOVERY) was published in the N Engl J Med past doctors of the United Kingdom [24, 25]. They plant that using dexamethasone (6 mg/day, one time daily for up to 10 days) reduced the number of deaths in ventilated patients by i-third, and in patients receiving oxygen therapy without mechanical ventilation, the deaths were reduced past one-fifth in adults patients with COVID-19. Notwithstanding, there was no benefit (and the possibility of impairment) in patients who did not crave oxygen therapy [24]. Simultaneously, our inquiry squad published a research result entitled "Glucocorticoids improve astringent or critical COVID-19 through activating ACE2 and reducing IL-6 levels" [26]. This research demonstrated that low-dose of methylprednisolone (40 mg/d if body weight ≤ 80 kg for the first 3-4 days, and and then 20 mg/d for the next 3 days or more with a total of less than 8 days) improved the clinical tests and chest CT images in 7 out of 9 patients of severe or critical COVID-19. We focused on the molecular target angiotensin-converting enzyme 2 (ACE2) of SARS-CoV-2 and screened a group of ACE2 agonists by bioinformatics. Glucocorticoids are a type of ACE2 activator. We further verified the efficacy of nine chemicals on regulating ACE2 expression in homo GES-one, an upper digestive tract epithelial prison cell line, and THP-1, a human being monocyte cell line, and plant that several glucocorticoids possessed activating effects on ACE2 in both cell lines. Our group likewise compared the efficacies of several glucocorticoids. Hydrocortisone showed the strongest effect on ACE2 activation, followed by prednisolone, and methylprednisolone [26]. Given their powerful anti-inflammatory and immunomodulatory effects, glucocorticoids are an obvious potential therapy for astute lung injury in severe COVID-19[27]. Along with the efficacy in treating the acute lung injury / acute respiratory distress syndrome (ARDS), glucocorticoids have been proposed as a life-saving drug for treating COVID-nineteen[25, 28]. On 2 September 2020, the standard treatment for severe or critical patients with COVID-19 was recommended by the WHO guideline (https://world wide web.who.int/publications/i/item/WHO-2019-nCoV-Corticosteroids-2020.i) (Fig. two). However, the limitation of RECOVERY written report is that the side furnishings of glucocorticoids are not fairly assessed.
Fig 2
The flowchart of changed insights for glucocorticoids used in the treatment of severe COVID-19 since the pandemic.
(View in new window)
Thereafter, the efficacy of glucocorticoids in the handling of COVID-19 has been reported by dissimilar groups from unlike countries [29-31]. Keller et al. reported that glucocorticoids could significantly reduce the risk of mortality or mechanical ventilation (odds ratio, 0.23; 95% CI, 0.08-0.70) if the initial level of C-reactive protein (CRP) is >/=20 mg/dl. However, using glucocorticoids would increment the risk of mortality or mechanical ventilation (OR, two.64; 95% CI, ane.39-5.03) if the CRP level is less than 10 mg/dl [32]. On v January, 2021, Chinese researchers proposed the utilise of glucocorticoids for COVID-nineteen treatment. They used the ratio of neutrophils to lymphocytes (NLR) as an evaluation alphabetize to decide the clinical efficacy of glucocorticoids. They analyzed 12,862 COVID-nineteen cases from 21 hospitals in Hubei Province, and establish that NLR > vi.11 at admission is a risk factor for mortality. Nonetheless, glucocorticoids treatment in such individuals is associated with a depression 60-day all-cause mortality. Conversely, in individuals with an NLR </= 6.11 or with type ii diabetes, glucocorticoids handling was non associated with reduced mortality, but rather increased risks of hyperglycemia and infections[33]. Recently, Liu and coworkers proposed that assistants of glucocorticoids in severe COVID-xix is associated with increased 28-24-hour interval mortality and delayed SARS-CoV-2 coronavirus RNA clearance [34]. Still, Ji et al. reported that glucocorticoid therapy does not filibuster viral clearance in COVID-19 patients [35]. To analyze the result of glucocorticoids on patients with severe pneumonia, Liu and colleagues institute that there was no pregnant departure between patients using low dose (</= 2 mg/kg mean solar day) and high dose (> 2 mg/kg twenty-four hour period) methylprednisolone in inhibiting IL-vi production. In that location was no significant difference in virus clearance between patients with and without methylprednisolone use [36]. Ai and coworkers proposed that glucocorticoids could be used in severe or critical illness. Co-ordinate to the experience of treating COVID-19 patients in Shanghai, the dose of methylprednisolone was 40-lxxx mg/day for iii days, and then reduced to twenty mg/24-hour interval, with a full treatment catamenia of less than 7 days. The side effects are minimum with this dose regimen [37].
Glucocorticoids and treatment of solid tumors
Glucocorticoids have been used in clinical oncology for over half a century for alleviating side effects induced by chemotherapy or radiotherapy. As a supportive therapy, glucocorticoids are frequently used for increasing appetite, reducing weight loss, eliminating fatigue, and preventing vomiting [38]. Glucocorticoids are likewise constructive in alleviating hurting associated with bone metastasis by inhibiting the synthesis and release of prostaglandins in advanced cancer patients [39]. However, a meta-analysis disclosed that the use of glucocorticoids should be avoided in patients with avant-garde cancers, because it may reduce survival of patients with lung cancer as palliative/supportive care purpose [40].
Currently, immune checkpoint inhibitor (ICPI) therapy used in cancer treatment exerts its effect by blocking the actions of cytotoxic T-lymphocyte-associated poly peptide 4 (CTLA-4) and programmed cell expiry protein ane (PD-1). ICPIs can heighten antitumor amnesty by blocking negative regulators of T-cell office that be on both immune cells and tumor cells. Although these agents tin can pb to remarkable responses, they are likewise associated with immune-related adverse effects (irAEs). Friedman and colleagues proposed that PD-1 inhibitors such every bit nivolumab and pembrolizumab take a lower incidence of irAEs compared with those that block CTLA-iv such as ipilimumab. The combination of nivolumab and ipilimumab has a college rate of irAEs than either approach as monotherapy. The most common irAEs include rash, colitis, hepatitis, endocrinopathies, and pneumonitis. The treatment of irAEs requires immunosuppression with glucocorticoids [41], because ICPI results in an increase of effector T cells, that respond to self-antigen, and pb to autoimmunity. The caste of autoimmune effect may be correlated with tumor response to immunotherapy. ICPI could enhance the anti-tumor effects of T-cells, just also heighten the immune response to normal tissues [42]. On October 2015, Horvat and colleagues reported their clinical findings in patients with melanoma who had received ipilimumab treatment at the standard dose of 3 mg/kg, and observed irAEs. Of the 298 patients, 254 (85%) experienced irAEs of whatever form, and 56 (xix%) discontinued therapy because of irAEs, most unremarkably diarrhea. A total of 103 (35%) patients received treatment with systemic glucocorticoids. They suggested that irAEs are common in patients treated with ipilimumab. Based on their experience, approximately one-third of ipilimumab-treated patients required treatment with systemic glucocorticoids [43]. Arbour and coworkers reported that there were 90(14%) of 640 patients of not-small-prison cell lung cancer treated with unmarried-agent PD-(L) 1 occludent who also received glucocorticoids of >/= ten mg of prednisone equivalent daily at the start of the PD-(L)i blockade therapy. The common indications for corticosteroids were dyspnea (33%), fatigue (21%), and brain metastases. They suggested that the baseline utilise of glucocorticoids >/= 10 mg of prednisone or equivalent was associated with poor outcome in patients with non-small-cell lung cancer who were treated with PD-(L)1 blockade. Prudent employ of glucocorticoids at the fourth dimension of initiating PD-(L)i occludent is recommended [44].
The 2-sided sword concerns of using glucocorticoids also existed in cancer handling. Taking the widely used dexamethasone equally an example, this drug belongs to the long-interim glucocorticoid, which has stronger anti-inflammatory, anti-allergic and anti-toxic effects than prednisone (mid-acting glucocorticoid). Thus, dexamethasone is only suitable for short-term usage. The long-term application of dexamethasone can lead to iatrogenic adrenal insufficiency [45]. In addition, if cancerous tumor cells overexpressed glucocorticoid receptor, using glucocorticoids should exist careful, because overexpression of glucocorticoid receptor may promote the proliferation of malignant cancer cells [46, 47]. Theoretically, the effects of glucocorticoids are mediated by the ubiquitously expressed glucocorticoid receptor, an intracellular ligand-activated transcription factor. Upon glucocorticoid binding, the glucocorticoid receptor becomes hyperphosphorylated. The hyperphosphorylated receptor subsequently migrates to the nucleus, where the glucocorticoid receptor can demark to DNA straight to regulate transcription of target genes [48]. Tian and colleagues analyzed the furnishings of expression of glucocorticoid receptor on colorectal carcinoma cell lines HT29 (master prison cell line) and T84 (metastatic cell line). They found that the expression of glucocorticoid receptor were significantly upregulated in nucleus of metastatic T84 cells. Dexamethasone treatment caused increased proliferation and invasion in T84 cell, compared to HT29 jail cell through activating CDK1 expression. Depletion of glucocorticoid receptor suppressed proliferation of metastatic colon carcinoma cells. Depletion of CDK1 too suppressed the proliferation and invasion of T84 cells. This study suggests that glucocorticoid- glucocorticoid receptor -CDK1 pathway induces proliferation and invasion of colon cancer cells [49].
On the other hand, some studies plant that glucocorticoids could suppress cancer proliferation through activating glucocorticoid receptor [l, 51]. For case, Yao and coworkers recently demonstrated that dexamethasone inhibits pancreatic tumor growth in preclinical models. They examined the expression of glucocorticoid receptor of two pancreatic cancer cell lines, PANC-1 and SW1990, and establish that arable expression of glucocorticoid receptor in PANC-1cells. Dexamethasone treatment significantly inhibited colony germination, migration, and tumor growth of PANC-ane cells. The underlying mechanisms involved in suppression of phosphorylation of nuclear factor κB and downregulation of epithelial-to-mesenchymal transition, interleukin 6 and vascular endothelial growth gene. Their findings suggest that dexamethasone effectively inhibits pancreatic tumor growth partially through activation of glucocorticoid receptor. The potential correlation between glucocorticoid receptor expression and anti-cancer efficacy of dexamethasone provided a new direction for developing target therapy [52].
In conclusions, glucocorticoids are important hormones in response to internal or environmental stresses. Nonetheless, chronic glucocorticoid use tin can result in detrimental side effects, including osteoporosis, hyperglycemia, diabetes mellitus, obesity, cardiovascular diseases and depression. Therefore, attention should be given on the dual roles of glucocorticoids. In patients with astringent or critical COVID-19, glucocorticoids are ideally administered for brusk-term use for their classical anti-inflammatory activities. Chronic and systemic apply of glucocorticoids should be avoided, considering they tin profoundly impact os jail cell function and mineral metabolism, and lead to osteoporosis [53]. Clinically, glucocorticoids may improve some symptoms, quality of life of patients with avant-garde cancer. However, the long-term glucocorticoid therapy in cancers is associated with adverse effects.
Table 1
Comparing of anti-inflammatory function, equivalent doses, plasma half-life and acting duration of several glucocorticoids
| Category | Drug | Event of anti-inflammation (ratio)* | Equivalent dose(mg)* | Plasma half-life (min.) | Duration of action(h) |
|---|---|---|---|---|---|
| Short-acting | Hydrocortisone | 1 | xx | 90 | 8-12 |
| Cortisone | 0.8 | 25 | 30 | 8-12 | |
| Mid-acting | Prednisone | iii.5 | 5 | 60 | 12-36 |
| Prednisolone | 4.0 | 5 | 200 | 12-36 | |
| Methylprednisolone | 5.0 | four | 180 | 12-36 | |
| Triamcinolone | 5.0 | 4 | >200 | 12-36 | |
| Long-interim | Dexamethasone | 30 | 0.75 | 100-300 | 36-54 |
| Betamethasone | 25-35 | 0.half dozen | 100-300 | 36-54 |
* The ratio of anti-inflammatory effects is measured past the reference of hydrogenation every bit 1. The equivalent dose is based on the hydrogenated as reference.
Acknowledgements
This project was partially supported by the Shanghai Scientific discipline and Technology Committee (20DZ2201900 and 18411953100) to YY, the Chinese National Key Program (MOST-2017YFC0908300 and 2016YFC1303200) to YY, the National Natural Science Foundation of China (82072602 and 81772505) to YY, and the Innovation Foundation of Translational Medicine of Shanghai Jiao Tong University School of Medicine (TM202001) to YY.
Competing Interests
The authors have declared that no competing involvement exists.
References
1. Vandewalle J, Luypaert A, De Bosscher M, Libert C. Therapeutic Mechanisms of Glucocorticoids. Trends Endocrinol Metab. 2018;29:42-54
ii. Timmermans S, Souffriau J, Libert C. A Full general Introduction to Glucocorticoid Biology. Front Immunol. 2019;10:1545
3. Alessi J, de Oliveira GB, Schaan BD, Telo GH. Dexamethasone in the era of COVID-19: friend or foe? An essay on the effects of dexamethasone and the potential risks of its inadvertent use in patients with diabetes. Diabetol Metab Syndr. 2020;12:80
4. Barnes PJ. Glucocorticosteroids: current and future directions. Br J Pharmacol. 2011;163:29-43
5. Adcock IM, Mumby S. Glucocorticoids. Handb Exp Pharmacol. 2017;237:171-96
6. Czock D, Keller F, Rasche FM, Haussler U. Pharmacokinetics and pharmacodynamics of systemically administered glucocorticoids. Clin Pharmacokinet. 2005;44:61-98
7. Daley-Yates PT. Inhaled corticosteroids: potency, dose equivalence and therapeutic index. Br J Clin Pharmacol. 2015;80:372-80
8. Bledsoe RK, Montana VG, Stanley TB, Delves CJ, Apolito CJ, McKee DD. et al. Crystal structure of the glucocorticoid receptor ligand binding domain reveals a novel way of receptor dimerization and coactivator recognition. Cell. 2002;110:93-105
nine. Pemmari A, Leppanen T, Hamalainen K, Moilanen T, Vuolteenaho K, Moilanen E. Widespread regulation of gene expression by glucocorticoids in chondrocytes from patients with osteoarthritis as determined by RNA-Seq. Arthritis Res Ther. 2020;22:271
10. Grbesa I, Hakim O. Genomic effects of glucocorticoids. Protoplasma. 2017;254:1175-85
xi. Escoter-Torres L, Caratti 1000, Mechtidou A, Tuckermann J, Uhlenhaut NH, Vettorazzi S. Fighting the Fire: Mechanisms of Inflammatory Gene Regulation by the Glucocorticoid Receptor. Front Immunol. 2019;10:1859
12. Mazzantini M, Di Munno O. Glucocorticoid-induced osteoporosis: 2013 update. Reumatismo. 2014;66:144-52
xiii. Vedamurthy A, Xu L, Luther J, Colizzo F, Garber JJ, Khalili H. et al. Long-Term Outcomes of Immunosuppression-Naive Steroid Responders Following Hospitalization for Ulcerative Colitis. Dig Dis Sci. 2018;63:2740-6
14. Russell CD, Millar JE, Baillie JK. Clinical evidence does non support corticosteroid handling for 2019-nCoV lung injury. Lancet. 2020;395:473-five
15. Shang L, Zhao J, Hu Y, Du R, Cao B. On the use of corticosteroids for 2019-nCoV pneumonia. Lancet. 2020;395:683-4
sixteen. Castelli Five, Cimini A, Ferri C. Cytokine Storm in COVID-19: "When You Come Out of the Tempest, You Won't Be the Same Person Who Walked in". Front Immunol. 2020;11:2132
17. Maskin LP, Olarte GL, Palizas F Jr, Velo AE, Lurbet MF, Bonelli I. et al. High dose dexamethasone treatment for Acute Respiratory Distress Syndrome secondary to COVID-nineteen: a structured summary of a written report protocol for a randomised controlled trial. Trials. 2020;21:743
18. Zhu HM, Li Y, Li Past, Yang S, Peng D, Yang Ten. et al. Effect of methylprednisolone in severe and critical COVID-19: Analysis of 102 cases. Globe J Clin Cases. 2020;8:5952-61
19. Borie R, Savale L, Dossier A, Ghosn J, Taille C, Visseaux B. et al. Glucocorticoids with depression-dose anti-IL1 anakinra rescue in astringent not-ICU COVID-19 infection: A cohort study. PLoS Ane. 2020;xv:e0243961
twenty. Callejas Rubio JL, Luna Del Castillo JD, de la Hera Fernandez J, Guirao Arrabal E, Colmenero Ruiz M, Ortego Centeno N. Effectiveness of corticoid pulses in patients with cytokine storm syndrome induced past SARS-CoV-two infection. Med Clin (Engl Ed). 2020;155:159-61
21. Sterne JAC, Diaz J, Villar J, Murthy S, Slutsky Equally, Perner A. et al. Corticosteroid therapy for critically sick patients with COVID-xix: A structured summary of a study protocol for a prospective meta-analysis of randomized trials. Trials. 2020;21:734
22. Qin YY, Zhou YH, Lu YQ, Sun F, Yang South, Harypursat V. et al. Effectiveness of glucocorticoid therapy in patients with severe coronavirus affliction 2019: protocol of a randomized controlled trial. Chin Med J (Engl). 2020;133:1080-6
23. Hu Y, Wang T, Hu Z, Wang X, Zhang Z, Li 50. et al. Clinical efficacy of glucocorticoid on the handling of patients with COVID-19 pneumonia: A single-center experience. Biomed Pharmacother. 2020;130:110529
24. Group RC, Horby P, Lim WS, Emberson JR, Mafham M, Bong JL. et al. Dexamethasone in Hospitalized Patients with Covid-19 - Preliminary Study. North Engl J Med. 2020
25. Ledford H. Coronavirus breakthrough: dexamethasone is showtime drug shown to relieve lives. Nature. 2020;582:469
26. Xiang Z, Liu J, Shi D, Chen Westward, Li J, Yan R. et al. Glucocorticoids ameliorate astringent or critical COVID-nineteen by activating ACE2 and reducing IL-6 levels. Int J Biol Sci. 2020;16:2382-91
27. Moore JB, June CH. Cytokine release syndrome in severe COVID-19. Science. 2020;368:473-4
28. Deng CX. Glucocorticoids save lives in COVID-19 patients. Int J Biol Sci. 2020;16:2477-8
29. Fernandez-Cruz A, Ruiz-Antoran B, Munoz-Gomez A, Sancho-Lopez A, Mills-Sanchez P, Centeno-Soto GA. et al. A Retrospective Controlled Cohort Study of the Impact of Glucocorticoid Handling in SARS-CoV-2 Infection Bloodshed. Antimicrob Agents Chemother. 2020 64
30. Han D, Peng C, Meng R, Yao J, Zhou Q, Xiao Y. et al. Estimating the release of inflammatory factors and use of glucocorticoid therapy for COVID-19 patients with comorbidities. Aging (Albany NY). 2020;12:22413-24
31. Fu HY, Luo Y, Gao JP, Wang L, Li HJ, Li X. et al. Effects of Short-Term Depression-Dose Glucocorticoids for Patients with Balmy COVID-19. Biomed Res Int. 2020;2020:2854186
32. Keller MJ, Kitsis EA, Arora South, Chen JT, Agarwal S, Ross MJ. et al. Effect of Systemic Glucocorticoids on Mortality or Mechanical Ventilation in Patients With COVID-19. J Hosp Med. 2020;15:489-93
33. Cai J, Li H, Zhang C, Chen Z, Liu H, Lei F. et al. The Neutrophil-to-Lymphocyte Ratio Determines Clinical Efficacy of Corticosteroid Therapy in Patients with COVID-xix. Cell Metab. 2021
34. Liu J, Zhang S, Dong X, Li Z, Xu Q, Feng H. et al. Corticosteroid treatment in severe COVID-xix patients with acute respiratory distress syndrome. J Clin Invest. 2020;130:6417-28
35. Ji J, Zhang J, Shao Z, Xie Q, Zhong L, Liu Z. Glucocorticoid therapy does not delay viral clearance in COVID-xix patients. Crit Care. 2020;24:565
36. Liu F, Ji C, Luo J, Wu W, Zhang J, Zhong Z. et al. Clinical characteristics and corticosteroids application of dissimilar clinical types in patients with corona virus disease 2019. Sci Rep. 2020;10:13689
37. Ai J, Li Y, Zhou X, Zhang W. COVID-19: treating and managing severe cases. Cell Res. 2020;xxx:370-i
38. Morrow GR, Shelke AR, Roscoe JA, Hickok JT, Mustian K. Management of cancer-related fatigue. Cancer Invest. 2005;23:229-39
39. Lin KT, Wang LH. New dimension of glucocorticoids in cancer treatment. Steroids. 2016;111:84-8
xl. Petrelli F, Bukovec R, Perego G, Luisa R, Luciani A, Zaniboni A. et al. Association of steroid use with survival in solid tumours. Eur J Cancer. 2020;141:105-fourteen
41. Friedman CF, Proverbs-Singh TA, Postow MA. Treatment of the Immune-Related Adverse Furnishings of Immune Checkpoint Inhibitors: A Review. JAMA Oncol. 2016;ii:1346-53
42. Marinelli D, Giusti R, Mazzotta Chiliad, Filetti M, Krasniqi Eastward, Pizzuti L. et al. Palliative- and not-palliative indications for glucocorticoids use in course of immune-checkpoint inhibition. Electric current testify and future perspectives. Crit Rev Oncol Hematol. 2021;157:103176
43. Horvat TZ, Adel NG, Dang TO, Momtaz P, Postow MA, Callahan MK. et al. Immune-Related Adverse Events, Need for Systemic Immunosuppression, and Effects on Survival and Fourth dimension to Treatment Failure in Patients With Melanoma Treated With Ipilimumab at Memorial Sloan Kettering Cancer Middle. J Clin Oncol. 2015;33:3193-8
44. Arbour KC, Mezquita L, Long N, Rizvi H, Auclin E, Ni A. et al. Impact of Baseline Steroids on Efficacy of Programmed Cell Death-1 and Programmed Expiry-Ligand one Occludent in Patients With Non-Small-Prison cell Lung Cancer. J Clin Oncol. 2018;36:2872-viii
45. Skov M, Master KM, Sillesen IB, Muller J, Koch C, Lanng Due south. Iatrogenic adrenal insufficiency as a side-result of combined treatment of itraconazole and budesonide. Eur Respir J. 2002;20:127-33
46. Zhidkova EM, Lylova ES, Savinkova AV, Mertsalov SA, Kirsanov KI, Belitsky GA. et al. A Brief Overview of the Paradoxical Role of Glucocorticoids in Breast Cancer. Chest Cancer (Auckl). 2020;14:1178223420974667
47. Ayroldi E, Cannarile L, Delfino DV, Riccardi C. A dual role for glucocorticoid-induced leucine attachment in glucocorticoid function: tumor growth promotion or suppression?. Cell Death Dis. 2018;9:463
48. Flaherty RL, Intabli H, Falcinelli M, Bucca One thousand, Hesketh A, Patel BA. et al. Stress hormone-mediated acceleration of chest cancer metastasis is halted past inhibition of nitric oxide synthase. Cancer Lett. 2019;459:59-71
49. Tian D, Tian M, Han G, Li JL. Increased glucocorticoid receptor action and proliferation in metastatic colon cancer. Sci Rep. 2019;9:11257
50. Dobos J, Kenessey I, Timar J, Ladanyi A. Glucocorticoid receptor expression and antiproliferative upshot of dexamethasone on human being melanoma cells. Pathol Oncol Res. 2011;17:729-34
51. Kostopoulou ON, Mohammad AA, Bartek J Jr, Wintertime J, Jung Yard, Stragliotto K. et al. Glucocorticoids promote a glioma stalk cell-like phenotype and resistance to chemotherapy in man glioblastoma primary cells: Biological and prognostic significance. Int J Cancer. 2018;142:1266-76
52. Yao Y, Yao QY, Xue JS, Tian XY, An QM, Cui Threescore. et al. Dexamethasone inhibits pancreatic tumor growth in preclinical models: Involvement of activating glucocorticoid receptor. Toxicol Appl Pharmacol. 2020;401:115118
53. Tang J. What can we acquire most corticosteroid therapy as a handling for COVID-19?. Osteoporos Int. 2020;31:1595
Author contact
![]() Corresponding writer: Yingyan Yu. Tel: (+86)21-34187336; Fax: (+86)21-64333548; Email: yingyan3yedu.cn
Corresponding writer: Yingyan Yu. Tel: (+86)21-34187336; Fax: (+86)21-64333548; Email: yingyan3yedu.cn
Received 2021-1-26
Accepted 2021-ii-24
Published 2021-four-x
What Are Glucocorticoids Used For,
Source: https://www.ijbs.com/v17p1530.htm
Posted by: lightliess1983.blogspot.com


0 Response to "What Are Glucocorticoids Used For"
Post a Comment